Expanded Review: Nutritional Status in Shoulder Arthroplasty Outcomes
Share
Shoulder arthroplasty, including total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA), has seen increasing utilization for managing degenerative and traumatic conditions. While advancements in surgical techniques have improved functional outcomes, postoperative complications and readmissions remain significant challenges. Emerging evidence identifies malnutrition, as measured by the Geriatric Nutritional Risk Index (GNRI) or hypoalbuminemia, as a modifiable risk factor strongly associated with adverse outcomes, including increased length of stay (LOS), readmissions, and mortality.(1,2,5)
Nutritional Status and Surgical Outcomes
Malnutrition and Complication Rates
A multi-institutional retrospective study found malnutrition to be significantly more prevalent among patients undergoing revision shoulder arthroplasty compared to primary procedures (36.6% vs. 19.5%). Malnourished individuals in this cohort experienced higher rates of pulmonary complications (10.4% vs. 6.6%), blood transfusions (11.3% vs. 1.6%), and an 18-fold increased risk of mortality.(1,3)
Additionally, a study in JSES Arthroplasty reported that patients with malnutrition undergoing revision TSA experienced significantly worse clinical outcomes, including a 1.8-fold increase in reoperation rates, 2.3-fold higher readmission rates, and 2.6-fold longer hospital stays compared to their well-nourished counterparts(4). These findings further underscore the necessity of early identification and intervention for at-risk patients.

Figure 1. Case selection schematic. TSA, total shoulder arthroplasty; NSQIP, National Surgical Quality Improvement Program; ASA, American Society of Anesthesiologists.(5)
Geriatric Nutritional Risk Index (GNRI)
The GNRI has emerged as a critical tool for assessing nutritional risk and predicting surgical outcomes. In a landmark study published in JSES International, patients with moderate malnutrition (GNRI 92–98) had a 1.9-fold higher risk of non-home discharge, a 3.4-fold increased mortality risk, and were 1.7 times more likely to experience any complication compared to those with normal nutrition.(5)

The risks were even more striking for patients with severe malnutrition (GNRI <92), who exhibited:
- A 3.3-fold increase in overall complications,
- A 9.8-fold increase in sepsis rates, and
- A 4.6-fold increase in mortality.
Severe malnutrition also significantly raised the likelihood of pneumonia (3.3-fold), extended LOS >2 days (3.3-fold), and readmissions (2.1-fold)(5). These findings highlight GNRI as a valuable tool not only for risk stratification but also for guiding preoperative optimization strategies to improve patient outcomes.
Cost Implications of Malnutrition
The financial burden of malnutrition in TSA is staggering. A study in the Journal of the American Academy of Orthopaedic Surgeons (JAAOS) revealed that one unplanned readmission in a bundled payment model offsets the profit from 55 uncomplicated TSA cases, translating to a net loss in bundled care profitability.(6)
Further analysis in the Journal of Shoulder and Elbow Surgery found that malnutrition independently increased total 90-day costs by approximately $5,850 per patient). The study also demonstrated that malnutrition significantly extended LOS (24.7% for moderate malnutrition and 41.6% for severe malnutrition, compared to 13.0% in the well-nourished group), contributing to higher hospital costs and resource utilization.(5,7)
The economic ramifications are further compounded by higher rates of complications and readmissions, with malnourished patients being 2.3 times more likely to require reoperation and 1.6 times more likely to be discharged to a rehabilitation or skilled nursing facility, further driving up costs.(7)
Conclusion
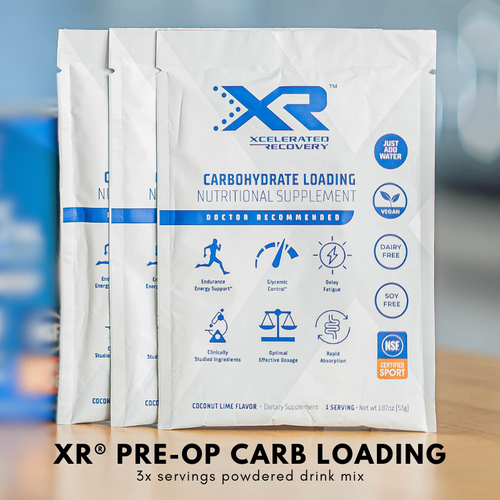
Malnutrition significantly impacts shoulder arthroplasty outcomes, increasing the risk of complications, readmissions, and prolonged hospital stays while placing a substantial financial burden on healthcare systems. The use of GNRI as a predictive and risk stratification tool is a promising strategy to identify and optimize at-risk patients preoperatively. Proactive nutritional optimization, including correcting hypoalbuminemia, implementing high-protein supplementation, and incorporating GNRI assessments into standard protocols, offers a path forward to improve clinical outcomes and align with value-based care initiatives.
Addressing malnutrition in TSA patients is not merely an opportunity, it is a necessity to ensure better recovery, reduced complications, and cost-effective care. Future research should focus on standardizing interventions and integrating nutritional management into comprehensive surgical prehabilitation programs.
References
- Garcia GH, Fu MC, Dines DM, et al. Malnutrition: a marker for increased complications, mortality, and length of stay after total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(2):193-200. doi:10.1016/j.jse.2015.07.034.
- Lee D, Lee R, Cross MT, et al. Low serum albumin levels are associated with increased 30-day cardiopulmonary complications, reoperation, and readmission rates following total shoulder arthroplasty. Iowa Orthopedic Journal. 2019;39(2):27-29.
- Flamant EM, Goltz DE, Burnett RA, et al. Malnutrition in elective shoulder arthroplasty: a multi-institutional retrospective study of preoperative albumin and adverse outcomes. J Shoulder Elbow Surg. 2021;30(11):2491-2497. doi:10.1016/j.jse.2021.03.143.
- JSES Arthroplasty. Malnutrition's impact on revision total shoulder arthroplasty outcomes. JSES Arthroplasty. Available at: jsesarthroplasty.org.
- Liu SH, Cerri-Droz P, Loyst RA, et al. The geriatric nutritional risk index as a strong predictor of adverse outcomes following total shoulder arthroplasty. JSES International. 2024;8(1):152-158. doi:10.1016/j.jseint.2023.08.022.
- Pezzulo JD, Farronato DM, Rondon AJ, et al. Predicting hospital readmissions after total shoulder arthroplasty within a bundled payment cohort. J Am Acad Orthop Surg. 2023;31(4):199-204. doi:10.5435/JAAOS-D-22-00449.
- Burns KA, Robbins LM, LeMarr AR, et al. Modifiable risk factors increase length of stay and 90-day cost of care after shoulder arthroplasty. J Shoulder Elbow Surg. 2022;31(2):1058-2746. doi:10.1016/j.jse.2021.08.010.