How to Beat Joint Infections Before They Start — and Recover Stronger If They Do
Share
Joint Infections: Prevention and Effective Recovery
The Crucial Role of Nutrition in Periprosthetic Joint Infection (PJI): Proactive Prevention and Enhanced Post-Surgical Healing
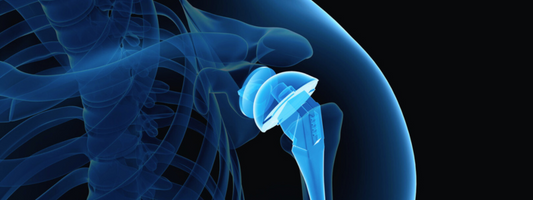
In joint replacement, implants, surgical technique, and sterile protocols get most of the focus. We are now recognizing the importance of a previously overlooked variable: nutritional status. Poor nutrition is not a secondary issue, it impairs immune function, delays wound repair, and increases failure rates in the management of periprosthetic joint infection (PJI).
Leading institutions and experts are now implementing better screening protocols, such as checking serum albumin and using validated tools like the Controlling Nutritional Status (CONUT) score and Geriatric Nutritional Risk Index (GNRI). These tools guide early identification of at-risk patients and support interventions including dietary strategies and targeted supplementation.

Evidence Linking Nutrition to Joint Infection Outcomes
Recent studies in Archives of Orthopaedic and Trauma Surgery, The Journal of Arthroplasty, Nutrients, and Journal of Shoulder and Elbow Surgery consistently show the impact of nutritional status on PJI outcomes:
-
Albumin <3.5 g/dL increased the risk of failure 5.6-fold after one-stage revision.
-
Poor nutrition (per CONUT score) raised the risk of two-stage exchange failure by nearly 9-fold.
- In revision THA for PJI, low albumin predicted higher reinfection rates and reoperation.
- In shoulder arthroplasty, preoperative malnutrition (albumin <3.5 g/dL, transferrin <204 mg/dL, or low leukocyte count) had markedly higher 90-day complications and increased 2-year risk of PJI (RR 2.0) and revision TSA (RR 1.8).
Poor nutritional status is common in PJI patients. Infection and inflammation further drive protein breakdown, creating a cycle of worsening nutritional reserves and poorer outcomes.
A Practical Framework for Clinicians
Nutritional status is a modifiable risk factor. Best practice now includes:
- Preoperative screening (albumin, CONUT, GNRI).
-
Targeted supplementation to address protein and amino acid deficits.
Personalized nutrition plans integrated into perioperative care.

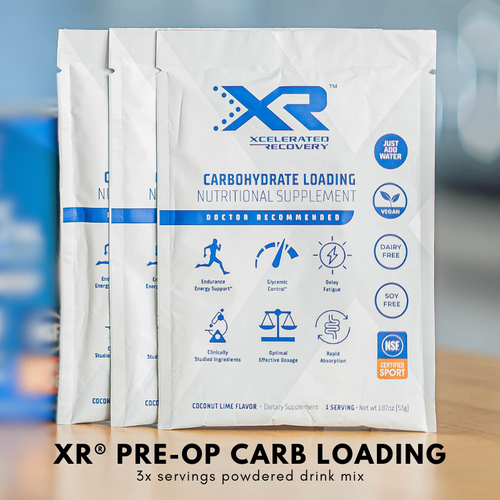
How XR® is Changing the Game with Nutrition-Based PJI Prevention and Recovery
Nutritional status is not just a lab value, it’s a modifiable risk factor. That's why our approach includes:
✅ Preoperative Nutritional Screening Guides:
✅ Targeted Supplementation:
✅ Personalized Nutrition Plans: Designed by clinical nutritionists personalized for each patient
Why This Matters for Surgeons and Clinicians
If you’re an orthopedic provider, you know how devastating PJI can be, for patients and for practice outcomes. Nutrition is one of the few modifiable risk factors that can directly impact infection control, surgical outcomes, and healthcare costs.
With growing evidence showing that:
- Failure rates remain as high as 25% in 2-stage revisions,
- Malnutrition is prevalent in up to 50% of PJI patients,
- And preoperative optimization may prevent complications,
Nutritional Optimization is a central part of PJI management protocols.

Why This Matters for Orthopedic Surgeons
-
Failure rates for 2-stage revisions remain as high as 25%.
-
Poor nutritional status is present in up to 50% of PJI patients.
-
Nutritional optimization reduces complications and improves infection clearance.
For patients, the message is clear: optimizing nutrition before surgery is one of the most controllable steps to improve recovery and reduce the risk of reinfection.
At XR®, our programs are specifically designed to help surgeons by providing evidence-based protocols and clinically studied supplementation programs in a simplified manner to help patients improve outcomes and decrease complications. We simplify evidence-based protocols and clinically studied supplementation programs to help surgeons improve patient outcomes and reduce complications.
References:
- Li Z, Maimaiti Z, Li ZY, Fu J, Hao LB, Xu C, Chen JY. Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection. Nutrients. 2022 Oct 21;14(20):4433. doi: 10.3390/nu14204433. PMID: 36297116; PMCID: PMC9607573.
- Traverso, G., Núñez, J.H., Gehrke, T. et al. Hypoalbuminemia increases the risk of failure following one-stage septic revision for periprosthetic joint infection. Arch Orthop Trauma Surg 143, 5641–5648 (2023). https://doi.org/10.1007/s00402-023-04885-z
- The Effect of Nutritional Status in the Treatment of Periprosthetic Joint Infections in Total Hip Arthroplasty Scarcella, Nicholas R. et al. The Journal of Arthroplasty, Volume 39, Issue 9, S225 - S228
- Green CC, Valenzuela MM, Odum SM, Rowe TM, Springer BD, Fehring TK, Otero JE. Hypoalbuminemia Predicts Failure of Two-Stage Exchange for Chronic Periprosthetic Joint Infection of the Hip and Knee. J Arthroplasty. 2023 Jul;38(7):1363-1368. doi: 10.1016/j.arth.2023.01.012. Epub 2023 Jan 21. PMID: 36693515.